2024 Author: Harry Day | [email protected]. Last modified: 2023-12-17 15:43
In the post-Soviet space, irritable bowel syndrome is still a diagnosis of exclusion. This means that a patient who complains of specific symptoms of gastrointestinal tract disorders is examined in every possible way, checking for all kinds of diagnoses, and without confirming any of them, IBS is determined. However, the main problem is that the patient is experiencing absolutely real pain, and the fact that the doctors did not find anything does not alleviate his condition, but only increases anxiety and, as a result, negative symptoms.
Psychosomatics of diagnosis. What is happening and how?
To begin with, it is worth noting that, as in all other psychosomatic cases, the stress factor finds a way out for each person in different organs and systems. It depends on heredity, and on constitutional characteristics, on environmental factors and the mental organization of a person, including, and even on upbringing, on the formation of attitudes regarding one's own body, and psychological trauma. If we take, for example, a situation of strong examination excitement, one student will experience dizziness, tachycardia, etc., the other, on the contrary, stomach cramps, the third excessive sweating, urge to urinate, etc. All this is due to the fact that each person reacts differently to the same stressful situation.
Moreover, the so-called fixation point of the symptom is also important. In one large-scale study of war veterans who suffered post traumatic stress disorder, irritable bowel syndrome only manifested itself in those soldiers who had some type of gastrointestinal disorder. We know that in neurosis, the psyche always uses more accessible ways to sublimate intrapersonal conflict. In this case, when there is an experience of experiencing gastrointestinal symptoms, the brain does not need to fixate on other less familiar symptoms and it follows the path of least resistance. This happens with almost any organ neurosis, be it cardioneurosis, bladder neurosis, hyperventilation, etc.
Vicious circle
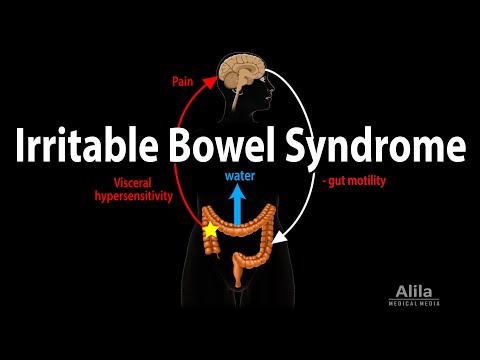
Let's not say now that if doctors have not confirmed a real disease, it can be various forms of anxiety or depressive disorders. Let us dwell on the fact that there is a "diagnosis" of IBS and now everything will follow the classic neurotic vicious circle.
1. We have a predisposition: naturally weak organs of the gastrointestinal tract; or a psychological traumatic memory associated with these organs; or metaphorical sublimation of the conflict (personal associations, psychotrauma); or problematic attitudes regarding our body, acquired in the process of education / formation, etc.
2. Further in our life there is some kind of complex conflict, stress, or some associations emerge from the memories that worry us. This becomes a trigger, a catalyst that triggers alarming symptoms of the autonomic system (the part of the nervous system that responds to adrenaline and innervates organs autonomously, regardless of our desires).
3. Vegetation reacts to stress, and the person fixates on the symptoms associated with the gastrointestinal tract.
4. The more anxiety about your condition = the more the autonomic system reacts with intestinal spasms and discomfort = the brighter the symptom and again the more anxiety. The circle is complete. Anxiety gives rise to a symptom, a symptom fuels anxiety.
Irritable bowel syndrome not hypochondria
Seeing the neurotic component in the problem, doctors may react in different ways. Some explain the problem, help manage stress, and prescribe symptomatic relief. And if the problem is "fresh", and everything is getting better in our life (the conflict has been resolved), this may be enough. Others disown the patient, arguing that it is all "in his head" or "it seems to him", hinting at hypochondria. Then it is more likely that the patient will really start going to the doctor to no avail, and the problem will only get worse.
However, in working with such clients, we can determine that with hypochondria, a person is sure that he suffers from some serious illness, goes from one specialist to another and undergoes unpleasant examinations many times. With IBS, the client may well be aware that this is such a diagnosis, come to terms with his symptoms, but what to do next, because he is really bad?
Psychological problems and comorbid disorders
It is important to remember here that although our symptoms are manifested in real pain and discomfort, their cause is still psychological. Moreover, the more we suffer, the more it affects our psyche and quality of life.
So, for example, due to the delicacy of the topic related to intestinal issues, most people are deprived of the opportunity to discuss their problems with loved ones openly. They find it difficult to explain changes in their behavior, which leads to misunderstandings, resentment and detachment. They gradually begin to withdraw into themselves, and being with a problem one on one can bring them to a state of despondency, hopelessness. Naturally, people have a decrease in self-esteem, self-confidence, and especially when comorbid (associated with the main problem) disorders, their quality of life begins to tend to zero.
Because of increased anxiety about their condition, people with IBS often become isolated from society. Since whether it is in transport, whether in a store, a place of study or work, having experienced a spasm, pain, etc., they begin to panic, associated with the fact that an attack of diarrhea will overtake them faster than they can find a toilet, or at any moment involuntary emission of gases can begin, and they disgrace themselves here and now. They refuse to travel and even just go to crowded places, places far from home, for fear of not being able to cope with their bodies. In order to minimize panic attacks or manage phobias, people with IBS create a variety of rituals to reduce anxiety. They think over routes taking into account the location of toilets, avoid transport and places where there is no way to urgently get to the toilet, take an unreasonable set of medications, become destructively picky about food, and may even switch to exhausting starvation. Especially many rituals appear in communication with loved ones and in the sphere of intimacy. And at the same time, the delicacy of the issue does not allow them to discuss their experiences with anyone. Fear, shame, hopelessness, anger towards oneself and one's body … so, imperceptibly, IBS absorbs a person and becomes the central experience of his entire life, and all mental and physical energy goes to fight him.
How to get rid of irritable bowel syndrome
As already discussed, in mild cases, the treatment prescribed by the gastroenterologist may well be sufficient to remove the symptoms and return to normal life.
If we are not talking about situational psychosomatics, but about the problem associated with the symptoms themselves here and now, and with psychological trauma, incorrect attitudes from childhood, constant stress, etc. - you cannot do without a psychologist-psychotherapist.
The methods of work can be different and depend on the history of a particular person.
Simply speaking out, getting support and feedback is a good start. However, further, it is important for someone to work with self-esteem and self-confidence, to understand their needs and to master the constructive skills of translating what they want. Determine your resistance to stress and find constructive ways to cope with stress and emotions. Someone should work out the issues of relationships with others, master communication skills, explore their psychological boundaries. For some, specific techniques of cognitive-behavioral therapy are more valuable, which will help to cope with anxiety and symptoms, to change some of the destructive attitudes. Sometimes it is extremely important to analyze the past, childhood, personal associations and the possibility of working through psychological trauma. In cases of heredity and constitutional predisposition, it is also important to understand the symptom, oneself in it and the methods of coping. And more often a combination of all of the above is needed.
If this history of IBS lasts for years, becomes overgrown with phobias and obsessions, the psychologist will recommend contacting a psychiatrist. Prescribed medications will help alleviate symptoms and make working with a psychotherapist more effective and productive.
Be healthy)
Recommended:
Loss And Grief. Article For Victims And Helpers, Self-help And Therapy

Loss and grief. Article for victims and helpers, self-help and therapy The article was written both for people experiencing loss, supporting loved ones, and for representatives of helping professions. Death, divorce, termination of relationships, social and financial "
"Psychosomatics" Is Not What You Just Thought! About Masks Of "psychosomatics", Norm And Pathology

From the reaction of some readers to my notes, I realized that many understand "psychosomatics" in no other way than a collective image of stories that "all diseases are from the brain." However, it is not. To explain, I have grouped my most frequent answers to questions about "
Three Stages Of Development Of The Victim Syndrome And The Point Of No Return

A small fragment of an article from the chapter on Victim Syndrome from the book "Notes of a Practicing Psychologist". For 12 years of work with psychosomatic and anxiety syndrome, I have accumulated a sufficient amount of material, a small part of which I will publish in this article.
Stress And Learned Helplessness Syndrome In Office Workers

Every office worker is familiar with such concepts as stress, emotional burnout, helplessness. We all know that this, together with a sedentary lifestyle and habits, leads to poor health and relationships with others. We spend the long-awaited weekend watching TV series, or we just do nothing and stare into space.
And Laughter And Tears And Therapy

This article is about the therapist's feelings in therapy. On the manifestation of feelings by the therapist. And, I think, there are no definite answers to the questions raised in this article. This article is about my own answers to them. I was completing short-term therapy with a five-year-old boy who did not know how to be friends.